Database Discovery is an extension to the traditional e-discovery approach using enterprise business data as a source of insight. Rather than limit yourself to documents, emails, and text messages in your discovery practice, you can add transactional data from enterprise systems like Salesforce, Oracle, SAP, Concur, and more. Read on for more details on a specific case where database discovery was pivotal in forming a data-driven defense argument.
Case Study: Large Rehabilitation Hospital False Claims Matter
A large Inpatient Rehab Facility (IRF) was charged with submitting false patient data to maintain their classification as an Inpatient Rehabilitation Facility (IRF) and bill the government at higher rates. The relator alleged that a conspiracy to improperly diagnosed and score patients abilities upon admittance, enabling the company to defraud the Medicare system for overstated rehabilitation outcomes.
Solution: The primary issue here was a large patient population involving hundreds of patients across many different facilities. The potential damages and penalties were in the hundreds of millions of dollars. The defense counsel would have to parse through hundreds of cases and find a way to demonstrate that patient admit scores had been consistently and correctly applied. The approach involved comparing Functional Independence Measure (FIM) scores of patients before and after their stay, and comparing to re-admittance rates to prove or disprove efficacy.
This approach leveraged the following platform capabilities:
- Demographic data – Because the case involved patients from all over the country, the defense normalized patient demographics against the demographics of people in the region itself – to enable a fair comparison of relative health across the population.
- Segmentation – Patient scores were analyzed and segmented across a number of factors including age, duration of stay, relative FIM improvement during their stay, FIM regression at readmittance, the existence of comorbidities or other health factors.
The result was a well-defined analysis of FIM coding trends across facilities – providing a data-driven segmentation of patients with which to support a fact-based explanation of FIM scoring admittance and discharge practices. Breaking down the patients into segments to reflect age and other comorbidity factors armed the attorneys with the depth and substance needed to defend the client.
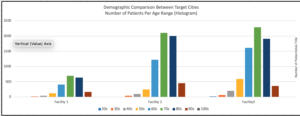
The FIM scores below show significant differences between the different facilities. However, the legal team was equipped to handle the discussion when the data was cross-compared with other demographic factors – such as the patient’s age in each facility, their average length of stay, and their FIM scores at entrance to the facility.
To learn more about this case and others where Database Discovery was employed, download our White Paper entitled: “Database Discovery: Extend Traditional E-Discovery with Enterprise Business Data.”
Sapling Data has more than 8 years experience building data analytics solutions and tools. Our Database Discovery platform enables legal and compliance teams to build a consolidated, cloud-based data warehouse for monitoring, investigation, and reporting needs.